Plantar Fasciitis
At some point in their life, most people will either suffer from, or know someone who is suffering from a type of heel pain called plantar fasciitis or plantar fasciopathy.
The source of the pain is initially caused by inflammation, followed by a prolonged degeneration of the heel bone ligament, called the plantar fascia.
Plantar fasciitis is the most common foot ailment that will prompt patients to see a GP or Podiatrist.
The symptoms include sharp, stabbing pains in the heel and is most noticeable when getting out of bed in the morning or when standing after a period of rest or inactivity.
Plantar fasciitis typically grumbles on for at least 6 months, and in some cases many years. Over time, many people with plantar fasciitis gradually alter their walking patterns, taking more weight along the outside of the foot and commonly avoiding placing too much weight directly through the heel itself.
Morton’s Neuroma
Morton’s neuroma on the other hand is a far less common condition, which causes a burning pain in the ball of the foot and toes. Sufferers experience numbness, pins & needles and sharp, stabbing pains in the forefoot, most commonly between the 3rd and 4th toes, and sometimes between the 2nd and 3rd toes.
The cause of the pain is degeneration and thickening of the small nerves that sit between the long bones of the forefoot; the metatarsals. When the thickened nerves reach a certain diameter in thickness they run out of space, leading to the nerve becoming squeezed and irritable.
Like plantar fasciitis, Morton’s neuroma sufferers gradually alter how they walk, choosing to slightly rotate the foot outwardly “pushing off” less forcefully through the ball of the foot.
Very little is known about the rates of cross-over, ie. how many people with plantar fasciitis will go on to develop Morton’s neuroma or vice versa.
However, we do know that there are a number of patients who are unlucky enough to have both conditions simultaneously.
What’s the link?
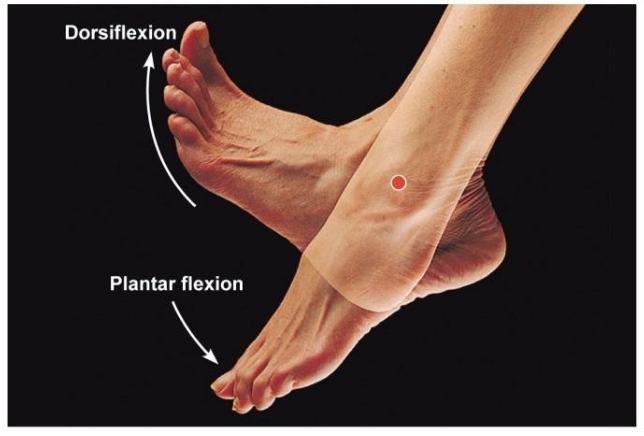
A common factor that can predispose a person to both conditions is a reduced ability to point the foot toward the shin bone, a movement known as dorsiflexion.
Normal ankle dorsiflexion values range between 0 – 20 degrees. Broadly speaking, the more ankle dorsiflexion you have the better, but as we age, we start to experience reduced ankle dorsiflexion.
This reduced ability often stems from tight calf muscles behind the lower leg. Such tightness impinges the ‘up-down’ hinge movement of the foot, causing the foot to adapt and compensate by performing the next best movement which is a ‘rolling in’ or ‘flattening’ movement of the longitudinal and transverse arches of the foot.
The rolling in movement (known as eversion) has long been associated with increased rates of Morton’s neuroma and plantar fasciitis.
Studies looking at both Morton’s neuroma and plantar fasciitis have shown reduced ankle dorsiflexion to be a big villain of the piece.
The single factor that chronic plantar fasciitis sufferers share is not age or weight but reduced ankle dorsiflexion. Reduced ankle joint dorsiflexion is found in a staggering 80-85% of heel pain sufferers.
It’s a similar picture for Morton’s neuroma; a 2016 study compared 68 patients with Morton’s neuroma to non-neuroma control subjects of similar age, weight, sex and foot type. They found that factors like foot type, foot shape, and body weight didn’t really seem to be significant in the formation of neuromas. The big factor that stood out like a sore thumb was reduced ankle dorsiflexion.
They calculated that the odds of developing Morton’s neuroma increased by a staggering 61% in the right foot and 43% in the left, for every 1-degree loss of ankle dorsiflexion (why there was such a difference between the right and left feet is the subject of another blog entirely).
Treating a combination of conditions
At The Barn Clinic treatment centres in London and Sheffield, we have performed cryosurgery for long term sufferers of both plantar fasciitis and Morton’s neuroma for over 12 years.
As such we have built up a vast amount of knowledge about causes and links between the conditions. Accordingly, we now regard reduced ankle dorsiflexion to be at least equal to, the risks of being overweight or wearing poor footwear.
In our experience virtually, every patient with either plantar fasciitis or Morton’s neuroma will experience an improvement in their symptoms if they regain a few degrees of ankle dorsiflexion with the appropriate exercises.
So, if you are doubly afflicted with both plantar fasciitis and Morton’s neuroma it is statistically highly likely you will have reduced ankle dorsiflexion, so you definitely should perform calf stretching. However, Morton’s neuroma pain will only be eased but never disappear with calf stretching alone.
Cryosurgery offers such patients a more permanent solution. For patients who developed plantar fasciitis after chronic neuroma pain we often find that after cryosurgery for Morton’s neuroma the heel pain will quickly resolve once the person starts walking more normally again.
For those patients who develop Morton’s neuroma pain soon after, or sometimes, a long time after experiencing plantar fasciitis, care must be taken separate out the two conditions from each other. This is because many people have small neuromas in their feet and luckily get no pain from them. Some studies estimate that just over half the population will have a neuroma, however, only a tiny percentage of people with a neuroma actually experience pain from them.
Sometimes we see patients that have been diagnosed elsewhere with both plantar fasciitis and Morton’s neuroma based on clinical examination, patient history and sometimes, imaging reports.
The difficulty is that sometimes plantar fasciitis can sometimes mimic the pain of Morton’s neuroma. This is because the thickened heel ligament can compress the nerves in the heel area that supply the forefoot.
When nerves become compressed they radiate pain forwards, and in this case into the ball of the foot. Unless the nerves around the heel ligament are carefully assessed for signs of entrapment a clinician could mistakenly attribute forefoot pain to neuromas (that are actually silent and causing no pain) and not the plantar fasciitis.
Accordingly, when we see patients with both plantar fasciitis and small Morton’s neuroma we have found that by treating and curing the plantar fasciitis only with cryosurgery that the forefoot pain previously thought to stem from Morton’s neuroma disappears when the plantar fasciitis clears up often as early as 3 weeks post cryosurgery.
To summarise
If you have both plantar fasciitis and Morton’s neuroma the take home message from this blog is:
- Ankle dorsiflexion exercises will help (email us for free advice exercise sheet).
- Plantar fasciitis that developed after a long history of walking awkwardly due Morton’s neuroma can clear following cryosurgery to the Morton’s neuroma only.
- Plantar fasciitis can sometimes mimic Morton’s neuroma pain. If you have been diagnosed with both conditions simultaneously you need careful assessment.
For more information please visit our sister website
